Most people think of diabetes as a condition that only affects people who are overweight. But that’s not true. Many people who appear lean or have a “normal” BMI still develop insulin resistance and type 2 diabetes. This condition, sometimes called lean diabetes, is becoming more common, especially among women in midlife.
How Common Is Diabetes in Normal-Weight Midlife Women?
In the U.S., diabetes in lean adults (BMI under 25) has been steadily rising, even as awareness about obesity-related diabetes has increased. Similar trends are seen worldwide. Asian populations, for instance, have higher rates of diabetes at lower BMIs, showing that body fat distribution and metabolic flexibility are more important than weight alone.
Women in midlife face additional risk because of hormonal changes during the perimenopausal and menopausal transitions. Estrogen helps regulate insulin sensitivity and body fat distribution. As estrogen declines, fat tends to accumulate around the abdomen, increasing visceral fat — the metabolically active type that raises insulin resistance. This can happen even if the scale doesn’t move much.
So yes, even a “skinny” woman can develop type 2 diabetes if her hormones, stress levels, or lifestyle choices push her body toward insulin resistance or pancreatic burnout.
How Hormones Influence Insulin Resistance
Hormones are key regulators of metabolism. When they shift, so does blood sugar balance. Here’s how:
Estrogen: Estrogen promotes healthy glucose uptake in muscle and helps keep fat storage patterns more protective (hips and thighs instead of the belly). As levels drop, muscle insulin sensitivity decreases, and fat tends to migrate to the abdomen, driving inflammation and insulin resistance.
Progesterone and androgens: When progesterone declines faster than estrogen, or when androgen levels rise, women may notice worsening insulin sensitivity. This can resemble what’s seen in PCOS, even if symptoms are milder.
Cortisol: Chronic stress and poor sleep elevate cortisol, which raises blood sugar and drives fat storage around the midsection. Persistent cortisol elevation can eventually wear out the pancreas.
Thyroid hormones: Low thyroid function slows metabolism, lowers energy production, and can make it harder for cells to respond properly to insulin.
These hormonal imbalances explain why some midlife women who are otherwise “healthy” and at a normal weight still experience blood sugar problems.

Want to create a custom longevity health plan?
You’re in the right place.
I can help you with a functional approach to midlife women’s health including hormone balance, gut health, autoimmune issues, bone health, heart health and more!
Top 5 Functional Lab Tests to Ask For
If you suspect your blood sugar might be out of balance, these five tests can give you the best insight into your metabolic health. The “ideal” ranges listed here are tighter than typical lab norms and reflect what’s considered optimal for longevity and metabolic flexibility.
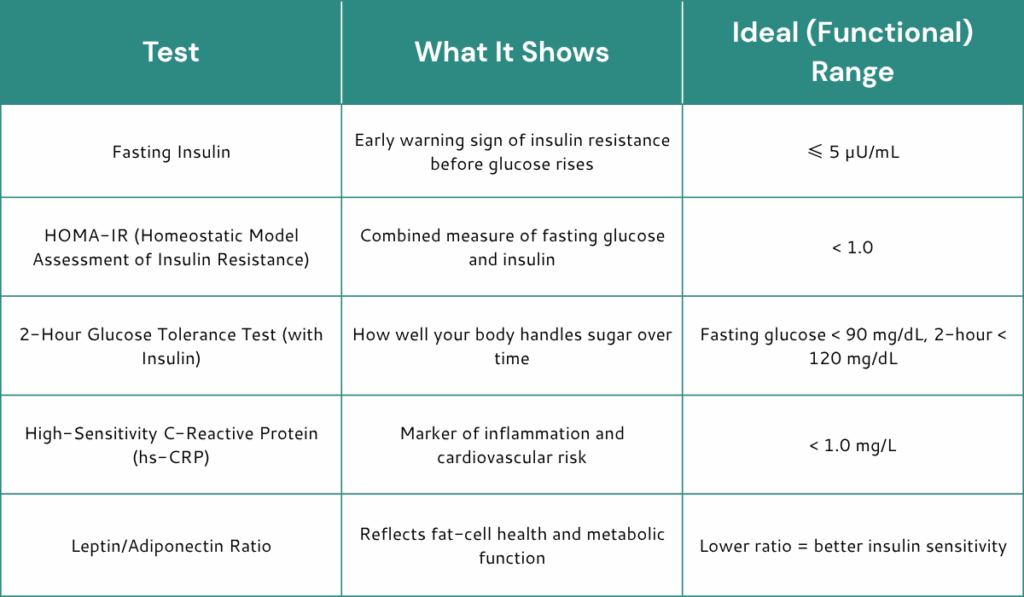
If you only run one or two of these, start with fasting insulin and hs-CRP. They’ll often reveal early problems long before fasting glucose or A1c rise out of range.
Lifestyle Strategies to Reverse or Prevent Diabetes
1. Build and preserve muscle.
Muscle is your biggest glucose sponge. Strength training two to four times per week improves insulin sensitivity and helps prevent the loss of lean mass that often occurs in midlife.
2. Time your meals.
Avoid grazing all day. Leaving 12–14 hours between your evening meal and breakfast supports metabolic flexibility and gives your insulin levels a rest.
3. Eat for blood sugar balance.
Focus on whole foods, plenty of vegetables, moderate protein, and healthy fats. Reduce refined carbs, added sugars, and processed foods. Include fiber at every meal to slow glucose absorption.
4. Prioritize sleep and stress reduction.
Poor sleep increases cortisol and insulin resistance overnight. Aim for 7–9 hours of restorative rest and practice mindfulness, yoga, or deep breathing to lower stress hormones.
5. Address gut health.
A healthy gut microbiome helps regulate metabolism and inflammation. Include fermented foods, fiber, and consider probiotic supplementation if needed.
6. Get daily movement.
Even walking after meals improves glucose control. Try “movement snacks” throughout the day rather than relying on one long workout.
7. Reassess hormone balance.
If perimenopause or menopause is contributing to symptoms, testing and addressing hormone imbalances can significantly improve metabolic health.
Helpful Supplements
Supplements aren’t magic bullets, but they can complement lifestyle work. These are some of the most well-researched and clinically effective for improving insulin sensitivity:
- Berberine: Supports insulin sensitivity and helps lower fasting glucose.
- Alpha-lipoic acid (ALA): Reduces oxidative stress and improves mitochondrial function.
- Inositol (Myo- and D-Chiro forms): Enhances insulin receptor activity and supports hormone balance.
- Magnesium (glycinate or malate): Involved in over 300 metabolic reactions, including glucose regulation.
- Chromium picolinate: Assists insulin in transporting glucose into cells.
- Vitamin D: Optimizing levels (40–60 ng/mL) improves insulin response and immune function.
- N-Acetyl Cysteine (NAC): Helps combat oxidative stress that worsens insulin resistance.
You can find professional-grade versions of these through my Fullscript store.
Diabetes, Longevity, and Why Numbers Matter
Even mild elevations in blood sugar or insulin shorten lifespan. High glucose accelerates aging by damaging blood vessels, nerves, and mitochondria. It promotes oxidative stress, inflammation, and the formation of advanced glycation end products — sticky molecules that literally make your tissues “stiffer” with age.
Women who maintain healthy insulin sensitivity generally enjoy better brain health, cardiovascular resilience, and energy in later years. The earlier you intervene, the easier it is to reverse insulin resistance and avoid complications.
Remember, “normal” lab ranges often represent the average of a very unhealthy population. Aim for optimal numbers, not just “normal” ones. Being proactive about your metabolic health now pays dividends for decades to come.
The Bottom Line
Yes, a skinny person can absolutely get diabetes. In midlife women, hormonal changes, stress, poor sleep, and low muscle mass can combine to create insulin resistance even without weight gain.
By focusing on strength training, balanced nutrition, stress management, gut health, and targeted supplementation, you can dramatically improve your body’s insulin response and protect your longevity.
Your weight might look “normal,” but your labs tell the real story. Pay attention to them. Prevention is always easier — and more powerful — than treatment.
If you’d like help creating a personalized longevity and hormone plan, visit www.drannagarrett.com/lets-talk.
References
Adesoba, T. P., et al. (2023). Trends in the prevalence of lean diabetes among U.S. adults. Diabetes Care, 46(4), 885–892.
Choi, M. J., et al. (2024). Menopause and diabetes risk along trajectory of β-cell changes. Healthcare, 13(9), 1062.
George, A. M., Jacob, A. G., & Fogelfeld, L. (2015). Lean diabetes mellitus: An emerging entity in the era of obesity. Diabetes/Metabolism Research and Reviews, 31(6), 518–527.
Kim, J. M., et al. (2024). Lean type 2 diabetes prevalence trends in Korean adults. BMC Public Health, 24, 21034.
Salvatore, T., et al. (2023). Current knowledge on pathophysiology of lean/normal-weight type 2 diabetes. International Journal of Molecular Sciences, 24(2), 2040.
Dr. Anna Garrett is a menopause expert and Doctor of Pharmacy. She helps women who are struggling with symptoms of perimenopause and menopause find natural hormone balancing solutions so they can rock their mojo through midlife and beyond. Dr. Anna is the author of Perimenopause: The Savvy Sister’s Guide to Hormone Harmony. Order your copy at www.perimenopausebook.com.
Dr. Anna is available for 1-1 consultations. Find out more at www.drannagarrett.com/lets-




